By KATRIANNA RAY
Capital News Service
LANSING — Michigan’s psychiatrist shortage is making mental health services hard to find in rural areas.
The state has roughly 11.84 practitioners per 100,000 residents, according to a study by the University of Michigan’s School of Public Health Behavioral Health Workforce Research Center.
That’s worse than the national average of 12.9 practitioners per 100,000 residents, according to the study.
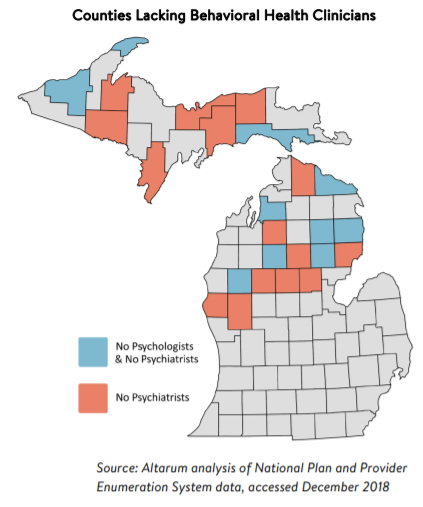
Six Upper Peninsula counties and nine Lower Peninsula counties have no psychiatrists, according to Altarum, a nonprofit health research organization in Ann Arbor. Three U.P. counties and seven Lower Peninsula counties have neither psychiatrists nor psychologists.
An even greater shortage exists within specialty practices, like addiction and child psychiatrists, it said.
Most practitioners are in the southeast part of the state, creating a disparity in services in rural areas, according to Professor Rajiv Tandon, the chair of Western Michigan University’s Department of Psychiatry.
“Rural communities are underserved,” Tandon said. “This is a problem that has gone on for a long time. If anything, it’s getting worse.”
Even though the salaries are high and the field is popular, many hospitals and mental health service centers lack the funding to have a psychiatry department, according to the study.
Developing programs that entice psychiatrists to move to rural areas, use of Telehealth services and strengthening residency ties to rural areas could help reduce such shortages.
It’s not an uncommon problem across the country. About 111 million people live in “mental health professional shortage” areas, according to the U.S. Department of Health and Human Services.
A majority of the 3,135 counties in the United States have no psychiatrists, the U-M study said..
The salaries for psychiatrists have gone up in the past few years, leading to a scarcity of job openings due to slower turnover, according to Tandon. Rural communities have fewer job openings as a whole.
“Interest in psychiatry in medical students has gone up and down over the last several decades,” Tandon said. “Over the last several years, it’s gone up. For example, we had more applicants to our residency program this year than in previous years.
“All the positions in psychiatry in the country have been filled. It’s a consequence of Obamacare, where the coverage for psychiatric services has received a higher priority,” he said.
The shortage of psychiatrists has spread already-thin resources and require many mental health practitioners to seek outside help, according to Christine Gebhard, the North Country Community Mental Health Authority’s chief executive officer. The authority, based in Petoskey, covers six counties: Antrim, Charlevoix, Cheboygan, Emmet, Kalkaska and Otsego.
“The shortage is very real. It limits access for patients, and it can create some wait time to get in for services, ” she said. “Many of us in this field use mid-levels, such as psychiatric nurse practitioners, who can do some of the same work of a psychiatrist,” Gebhard said. In addition, the authority uses primary care physicians to do some medication reviews and support work but not necessarily do psychiatric evaluations.
Another resource is Telehealth, a service that connects patients and clinicians over long distances. It allows contact, care and monitoring without the patient traveling long distances to a medical office, she said.
There is a strong correlation between where psychiatrists practice and where they completed their residency.
More than half of those who completed residency training between 2007 and 2016 practice in the same state, according to the Association of American Medical Colleges.
Western Michigan University’s Tandon said affiliations with academic psychiatric programs could create an incentive to practice in rural communities..
“We need to provide better incentives to work in those areas,” Tandon said. ”Providing the structure and the sense of belonging in a greater community of psychiatrists would be helpful,” he said.