From large healthcare facilities such as Beaumont Hospital and Bronson Hospital, to nursing homes and elective surgery, health care workers continue to bear the burden in Michigan where cases are rising higher than any other state.
Increasing COVID cases in hospitals
Southeast Michigan
Beaumont Health is the largest health care system in Michigan, servicing Southeast Michigan with eight hospitals. Last Thursday, April 15, Beaumont announced that its Royal Oak location is at maximum capacity with COVID-19 patients.

Lisa Muma, a nurse navigator for Beaumont Children’s Pediatric Oncology Long-Term Follow-Up Clinic, at Royal Oak Beaumont, said the pandemic has impacted all aspects of the hospital, underscoring how critical it is that as a community we remain understanding toward those at higher risk.
Muma’s clinic at Beaumont had to remain open throughout the pandemic, as the type of work her clinic performs can not be postponed. New procedures were put in place, so that the clinic could still safely operate.
“We are all wearing masks as well as eye protection (goggles), which can be scary to the patients since we are a pediatric clinic,” said Muma. We spent extra time helping the children understand why we are wearing masks and goggles to try and help them be more comfortable.”
Battle Creek
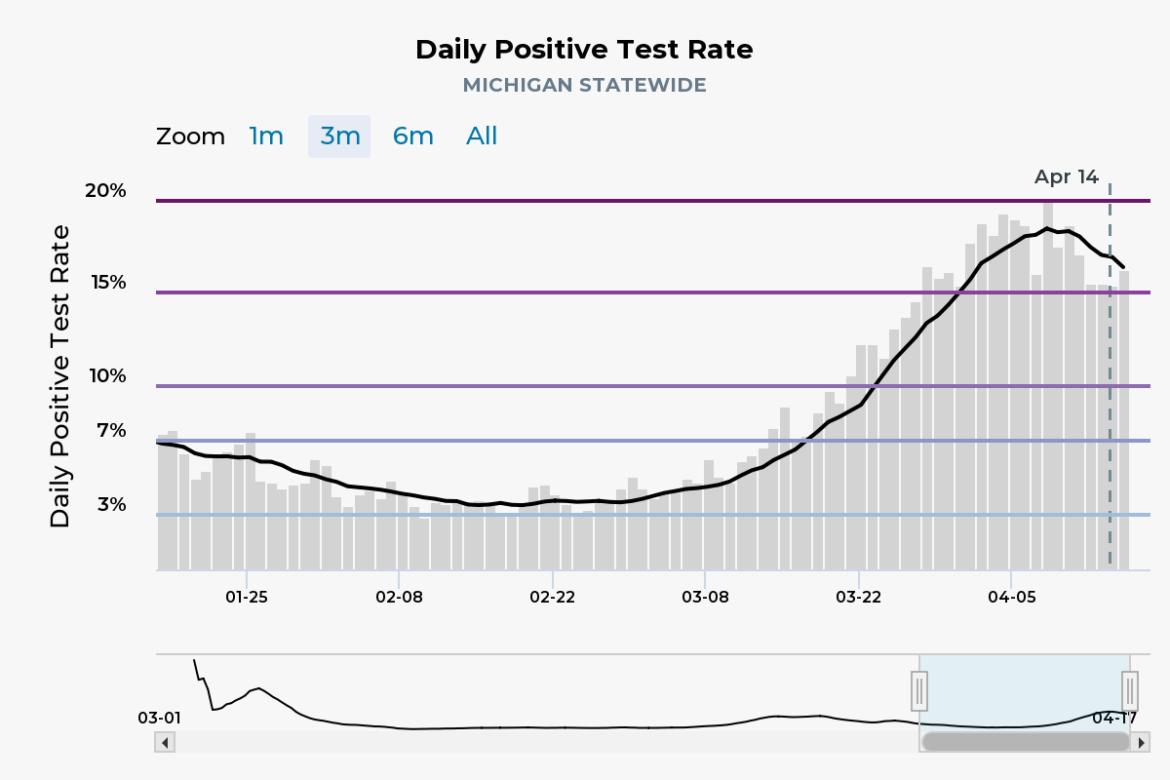
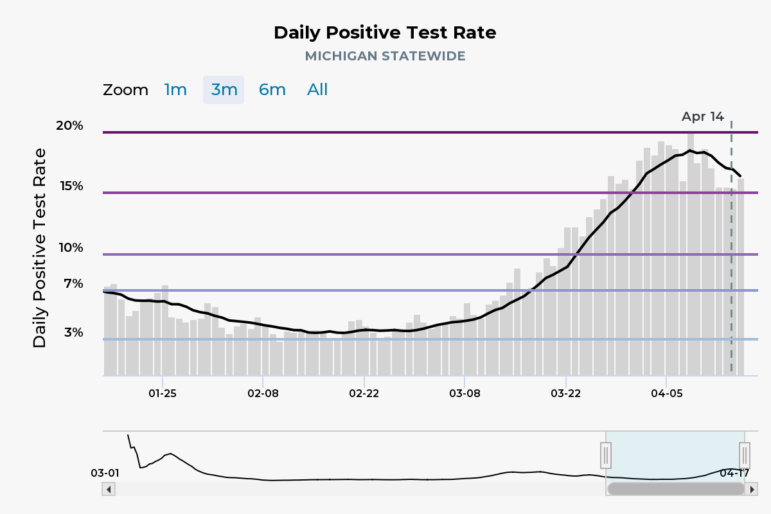
Calhoun County remains one of the fastest-growing hot spots for COVID-19 in the state of Michigan. According to the Centers for Disease Control, as of April 17, Calhoun County had a total of 12,624 people infected with COVID-19; that’s the third-highest among southwest Michigan counties.
On April 5, The New York Times reported that Battle Creek, located in Calhoun County, was the 8th-highest city in new cases reported. The ranking factored in the number of cases related to the size of the metropolitan area. New York City was ranked 7th. The numbers have since improved, but Battle Creek and Calhoun County are still among the highest number of cases in the state.
Bronson’s Guidelines
Bronson Battle Creek is the largest hospital in the county with 228 total beds.
“When our patient volumes change throughout the day, we make adjustments as needed,” said Carolyn Wyllie, a Bronson Healthcare spokesperson. “If we reach temporary capacity in certain areas, we may temporarily close to regional patient transfers or go on diversion to ambulance traffic until our capacity opens back up.”
“If we reach a level where our capacity is consistently above our normal licensed bed count or more than our current staffing model is designed for,” Wyllie added, “we will evaluate the need to implement our surge plan. This may include alternative staffing models and/or the addition of more beds, which were approved for emergency use by the state during the first phase of the pandemic.”
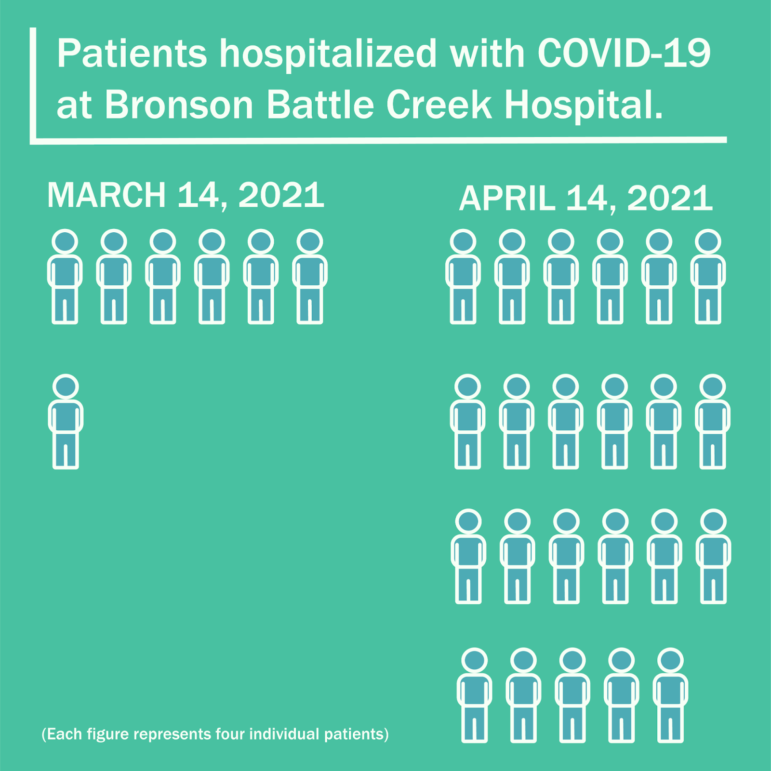
On April 10, Bronson Health Group made a change to its guidelines regarding visitors, prohibiting them outside of certain exceptions. Such exceptions include the Nursery, End of Life, and Emergency patients who are 18 or younger, have chronic impairments, or are critically ill, among others. The full list can be found on Bronson’s website.
Patients entering the hospital as well as potential visitors are screened for COVID-19 upon entry, with designated treatment areas for those who are positive or exhibit symptoms.
Bronson also offers vaccinations and testing to those in the area, with appointments and location information available on their website.
COVID for higher-risk patients
Linda Keilman, a gerontology nurse practitioner and associate professor in the College of Nursing at Michigan State University, takes care of older adults ages 50 and up in a nursing home.

“Nursing homes have been the hardest hit across the nation just because older adults who live there have many chronic conditions and they are very vulnerable,” Keilman said.
Keilman said extensive amounts of PPE had to be worn by her and her colleagues, such as face masks, goggles, disposable gowns, booties and gloves. Every three days, they took COVID-19 tests to make sure that they were negative.
“There were unimaginable levels of anxiety and stress,” Keilman said. “Worrying about whether you had come in contact with someone with COVID, worrying about bringing it in to the patients, worried about taking it home. It doesn’t give you a sense of security, which translates to some anxiety with taking care of the residents and patients at hospitals.”
Life changed for the residents at the nursing home as well. They had to mostly stay in their rooms and had to social distance from other residents. Additionally, their family members were no longer allowed to visit.
Allison Cronin, a nursing student, works at The Oaks. The Oaks is a senior living facility in Grand Blanc just outside of Flint.
“COVID continues to affect residents not just physically, but also mentally and emotionally. We aren’t allowed to have visitors in the facility so families have to come to the resident’s windows to talk to them,” said Cronin. “It’s very hard on the residents not being able to be close to their families and loved ones for over a year.”
A lot of nurses felt like they themselves couldn’t visit their families.
“One of the male nurses slept in his truck for a few weeks because he didn’t want to go into the house and affect his wife or his children,” Keilman said. “He was so dedicated to his role in taking care of others.”
He wasn’t the odd one out. For nurses around the world, this is part of the job.
“For nurses, patients are the most important,” Keilman said. “So when we become nurses we understand that our role is to give safe quality care for our patients, anytime, anyplace.”
Dr. Michael McLeod, endocrine surgeon at Sparrow Hospital and professor of surgery at Michigan State University, said that since the start of the pandemic, his patients have had to wait longer for their operations.
“We have had to develop a command team to make decisions on whether elective surgeries can continue or not based on what resources are required to care for hospitalized COVID patients,” McLeod said.
Effect on healthcare workers and how to help
The COVID-19 pandemic has taken a major toll on frontline workers, such as Danielle Woody, a nurse at Bronson Battle Creek.
“The pandemic stopped a lot of the traffic we saw coming to the hospital, including family and visitors,” Woody said. “That to me is one of the saddest things. When people are sick they need that support from friends and family.”
Woody also said she has felt unsafe .
“When the pandemic hit, all of our protective equipment started to disappear, and we had to ration all of our supplies,” she said. “Knowing that there were times we might not be safe is one of the scariest moments of my life.”
Carolyn Wyllie stressed the impact this all has had on frontline workers, and provided advice on what the public can continue to do to help slow the spread of the virus.
“It is important to recognize the strain this puts on our providers, nurses, and other front line staff members when patient volumes are as high as we’ve been seeing in recent days,” Wyllie said. “They continue to show great care, compassion, and dedication to the well-being of all of our patients and each other.”
“The best way to assist the medical community is to help slow the spread of COVID-19 by wearing a mask, social distancing, limiting gatherings and schedule an appointment to get vaccinated as soon as possible,” Wyllie added.
Muma asks that the community do its part in mask-wearing, stressing that while some may not feel at risk, there are still thousands of others in our communities who are very at risk.
“The way that your community can help our hospitals and show our support to staff is to wear those masks properly, covering the nose and mouth at all times when outside of your home,” said Muma.